I realized, after finishing the last very long post, that I didn’t actually go into my originally planned description of the Augusta trip. However, I began writing it in the days leading up to the second on-treatment scan. In the gap between working on it furiously on the plane en route to Memphis and being able to return to it, the scan itself took place. With a lot of anxiety around this milestone, Dr. Gajjar was quite careful in showing me two areas on the spine that might be of potential concern and that he had brought up with the radiologists. These were nothing worrisome, one being clearly a blood vessel (even to me), but he wanted to make sure I saw them before I went on my merry way. With some relief, we started disseminating the news of the all-clear and Colin and I returned to the Tri Delta House to relax before dinner with friends. However, the phone rang in our room and I was met with the familiar voice of Katie, a nurse who had taken care of Colin often when he had inpatient and now works in the brain tumor clinic. We needed to return to the hospital, which meant only one thing.

After the fretting over the spine, I assumed it was a spinal lesion, but it was not. Dr. Gajjar, frustrated that somebody had turned off the computer, grumbled as he went through the process of getting everything started back up and we waited in aggravated silence for more stomach churning minutes. There was no point in conversing over something that would begin glowing at us from that
bank of screens in short order. I did ask, “The spine?”
“No, ventricle,” Dr. Gajjar responded. And there it was, another pea, smaller than the one removed in February and tucked into the end of the lateral ventricle on the right side. And another, in the same ventricle but higher up. And then another blip, too vague to be definitively a tumor, which Dr. Gajjar had evidently pointed out to the radiologist; in the absence of the others, it might be a radiological artifact, easily ignored until the benefit of retrospect and a subsequent scan showed a clear lesion in the same spot. Now, everything looked like an incipient tumor. According to Dr. Gajjar, at this point, the radiologist panicked and started finding potential tumor everywhere. By his retelling, he cautioned the radiologist (and by transitive property me) to calm down.
We had anticipated the growth of new lesions as a possibility and already had a back-up plan ready. I say we, but I really mean Dr. Johnson, who had already included the potential for more surgery and radiation in the single patient IND. This means that we can address new lesions in various ways while staying on a version of the existing treatment course.
However, any significant change to the plan deserves careful consideration of all the available options. In preparation for this contingency, I had already met with Dr. Merchant, the radiation oncologist who crafted Colin’s original radiation plan, to discuss his current protocol for reirradiation of recurrent ependymoma. This would mean craniospinal irradiation (CSI) because of the metastatic disease. Now, with these additional lesions, there was no mistaking that this was truly metastatic, not just a single stray cell kicked off during one of the messy surgeries (even if that had been its genesis, the cancer has found its way into the broader system and could be expected to lurk anywhere in the central nervous system).
Pseudoprogression?

One of the possibilities with immunotherapy treatment that we understood early on was that of pseudoprogression. When immune cells attack a tumor, they occupy it and cause it to swell. This can cause a radiographical increase in size that isn’t actual growth. For a tumor too small to be seen on an MRI, it could mean the sudden appearance of a lesion. This, Dr. Johnson had warned us early on, was a possibility that we would deal with.
After four cycles and more than four months because of chemo-related delays, could this be pseudoprogression? Probably not, but possibly so. The regimen could be working on some parts of the disease but not others.In all probability, this is not pseudoprogression, but only a biopsy would tell us that, underscoring the value of another resection and a surgeon’s eye (and microscope).
Radiation and the Abscopal Effect
Our initial salvage plan was to use stereotactic radiosurgery, which has a very limited treatment field and doses chopped up into just a few days, compared to the 30+3 treatments that Colin originally got, followed by a continuation of the indoximod–temozolomide treatment he has been on since March. In mice, the radiation was even more effective than the chemo alone with the indoximod, so we always knew that this could be effective even if the initial treatment failed.
In theory, this may be due to something called the abscopal effect, a phenomenon seen with some cancers where radiation applied to one lesion appears to cause other untreated lesions to also disappear. This is surmised to be a response of the immune system, which begins assaulting the other tumors once it is activated and recognizes them as targets. Some are already experimenting with this effect in different adult tumors; this is the approach they are using for President Carter’s melanoma brain metastases, though they are using a PD-1 inhibitor which targets a part of the immune pathway further downstream from IDO.
This was the strategy we had in our back pockets going into the scan, the emotional security blanket that reminded us that things were okay, that we had a back-up on hand. However, we also knew that there is much more to a scan than a simple determination of thumbs up or down.The specific circumstances of progression would also guide our further decisions, and we knew that everything had to be on the table, even CSI.
Opinions and Decisions, Round 2
Colin’s case needed to be reexamined with the new information of the progression. For Dr. Merchant, the answer was simple: CSI. He has supportive data based on a retrospective study on reirradiation of ependymoma and told me during our consult that it can be “curative” (his word, not mine). Dr. Gajjar, when I repeated this to him, shook his head: “CSI is not going to cure Colin.”

“I know,” I told him. Colin has more strikes against him than we could have known before the surgery in March. The tumor that came out then was unsurprisingly similar to the original lesions removed in 2009/2010. However, there is one particular new test that St. Jude has added to ependymoma pathology analysis that I didn’t sufficiently appreciate until starting up research in the wake of this progression news: 1q gain, a chromosomal abnormality. This is the only chromosomal abnormality strongly correlated with prognosis, and it’s profound. Ependymoma has been divided into a number of major sub-types, and within three of the four malignant pediatric sub-types, the 1q gain is associated with worse prognosis. Colin is already assumptively in a poor prognosis sub-type, Posterior Fossa A (PFA), which typically occurs in younger children and has much more aggressive characteristics with higher relapse rates. At the five-year mark, two-thirds of PFA kids have relapsed. Add the 1q gain on top of that (as well as the involvement and magnitude of the original tumor), and it’s a miracle that he’s gone this long without relapse. The kid really does have good bad luck.
Although we did receive the 1q results along with the pathology results from the last surgery in March, we didn’t recognize the significance of that information at the time, and that awareness wouldn’t have changed anything; the best article I’ve seen on it came out in May, and it was only after the progression that I scrutinized it and really looked at that part of Colin’s pathology from St. Jude. We also never had a conversation with anybody at the hospital about it, and it wouldn’t have changed our approach, since we were already on our way to Augusta with a treatment plan at the time.
One has to be careful with data not to place inappropriate value on it; the results of these studies are collated from various institutions that may not have consistent treatment approaches, particularly with younger patients where judgment (and competence) on surgery and radiation can differ radically. Therefore, the outcomes for the younger kids may be skewed by incomplete resections or reluctance to use radiation, which is particularly relevant for the PFA population.Even so, Dr. Gajjar said that the St. Jude data alone, where treatment was consistent, showed a distinctive disadvantage for those children that was magnified for those with the 1q gain.
Now, I don’t have the data to pull apart myself and see if there was ever a child like Colin, with such a late relapse, etc. to determine whether the idea of a durable remission is possible, if there is some sliver of kids who make it despite these prognostic obstacles. There is always the possibility of an anomaly, even without one child tucked in the data. I do know that I corresponded with one of the authors of that May article, who is certainly more familiar with the underlying data and described Colin’s situation as “grave” (pun not intended but morosely relevant) and recommended that we pursue stereotactic radiosurgery if possible.
As I left the Star Trek room with Dr. Gajjar, he offered his support in any way possible and promised to email Drs. Boop and Merchant to solicit their opinions before leaving for a trip. The next day, minutes after sending Dr. Merchant a follow-up email, I literally nearly ran into him outside of Kay Cafe. He expressed concern that what we see in the MRI does not reflect what is really happening in the ventricles. If you open it up, he warned, you’re likely to find much more disease that you can’t see on the MRI. Do radiation. You can do surgery later, but he needs CSI if we have any chance of catching this disease and offering Colin the prospect of long-term survival, though views on the reality of that goal clearly differed.
The opinion was quite clear, but it also came from a man who focuses on maximizing cures while tolerating a lot of side effects in that pursuit. Knowing what I do about the impact of CSI on children, even though Colin is “older,” I remained apprehensive. What of the side effects, especially given Colin’s history of prior irradiation? His original tumor was quite large and required a boost around the brain stem, and then there is the fact that he suffered significant neurological damage from surgery that took years to overcome. The primary focus on the effects of CSI centers around cognitive effects, which alone are not pretty. At his age, we could expect to see him lose around 4 to 6 IQ points per year; in the short term, this would not be a big deal.
I am acutely terrified of Colin losing the ability to swallow after having gone down that road once before and knowing how important eating is to Colin’s quality of life. I also care about his hearing; as a social child and an auditory learner who is already deaf on one side with serious hearing impairment on the other, his hearing is crucial for interaction. Just the relatively short time following our visit that he must go without his hearing aid, which has been sent to the company for its annual cleaning, he has asked for it back several times and misses the auditory clarity it brings. How much would radiation steal from who Colin is, and how long would it take for that to have an effect?
Many years ago, my father entered a nursing home after hip surgery. At first blush, it seemed like a depressing holding pen for abandoned people who were gradually losing their faculties, and I often heard visitors exclaim that they would never allow themselves to end up in such a place, yet who was I to question their quality of life? What measure do we have? As people lose their abilities, do they wallow in grief at the loss or do they allow the bar to slide down to accommodate the change?
My experience then taught me that I cannot judge the quality of life of another, yet here I find myself making treatment decisions for a child based on these very questions. When we first entered the brain tumor world, I faced the reality that my child as I knew him, along with all my expectations for his future, were gone. I had to embrace whatever it was he would become. The bargains we make, for hearing, for mobility, and many other things, are not true deals with the devil. They are not exchanges, traded openly, if deceitfully (the devil drives a hard bargain). They happen and we accept them, and the only measure you are left with as a parent is a very basic one: is my child alive and here to love?
Is this not a selfish goal to some extent, or at what point does it cross a line? The myopia of early diagnosis and treatment give us a singular perspective that lacks the benefit of a more nuanced understanding of the brain tumor world. I stand without judgment of the families who have made these difficult decisions in favor of the uncertainties of an impaired survival, even knowing that treatment may bring with it a panoply of disabling deficits.I understand the desire to take great risks and face terrific uncertainty to achieve a cure; one often hears in cancer circles that parents should be happy to deal with the hassles of long-term side effects because that means that patient is still here to have them. We ourselves have had no complaints with Colin’s various side effects, from the daily growth hormone injections to the amorphous management of school and learning issues.
Keeping an Eye on the Prize
That said, after everything that Colin has gone through, it is extremely difficult for us to consciously put him in the position of suffering injuries that may change him and his quality of life in a meaningful way, especially when the trade-off is not a reasonable chance at a good quality survival. We know that the deck is stacked against him, so we choose quality of life over quantity. The mindless pursuit of durable remission, cure, or whatever you want to call it, can cause families to set aside concerns of the life lived today in exchange for the long view. We have the benefit of the hindsight of others who have walked this path before us and wished they had spent more time focusing on the immediacy of life rather than the extension of it, especially when the long view exists primarily in fantasy and conjecture.Theoretically, durable remission remains a distant possibility, but it is not one that we are willing to pay a high price for.
Bluntly put, this is an impossible line to navigate. The best we can hope is to stay close to the mark, to gather up enough information to make an informed decision, and attempt to stage treatments and interventions appropriately on Colin’s behalf in a game of block and tackle against ependymoma. These are all moving targets that shift with available options, changes in his condition, and our understanding of the disease that now is showing itself to progress like a juggernaut, sending out tiny but disruptive messengers with an unproven yet certain appetite for growth.
We have not, nor will we ever, give up on Colin. However, our definition is not one of a dogged pursuit of cure, as it is often interpreted, but of giving him the best opportunity for a life he deserves reflecting the realities of his situation. The specific goal is constantly changing to reflect the contemporaneous situation. Our job is not to keep him alive but to give him a life.
Early on in the course of the disease, we knew that his best shot for long-term survival was through a gross total resection followed by radiation. With what was known at the time, this was more important than tumor grade; that fact is still true, but science has given us a better idea of the types of cases where this approach alone is more often going to fail.
When Colin was two, and we were approaching this disease for the first time, we took tremendous risks in the pursuit of durable remission. I still shudder to think of the decision to proceed with the terrifying surgery that ended up neurologically devastating him. It could have been much worse, which we knew, but it was bad enough as it was; had this disease behaved more aggressively at the time, he may have been overtaken by ependymoma without getting the opportunity to have a childhood. This thought still haunts me today.

Though we know that Colin was able to squeak through and recover most of his faculties, the decision to proceed with that surgery still troubles me, and expending any mental energy contemplating it gives me vertigo. Small differences in his course and he might not have been so lucky. Hindsight is useless when you know that the trajectory of things could easily have swung the other way, leaving us as parents and decision makers both bereft and racked with guilt.
Had we known then what we do now, that our child had been dealt one crappy hand after another (insidiously involved tumor;PF-A; 1q gain), would we have sanctioned an aggressive surgery? I cannot paint a definitive picture of this thought experiment, but it is certainly plausible that we would have approached the second surgery differently. Depending on the ensuing results (there are still many outcomes that spill out from that decision), it is possible that we would never have come to know Colin as he is today; he would never have gotten to live the life that he has. None of these questions has a satisfactory answer, none of the decisions a satisfactory result.Every analysis can be twisted on its head and reinterpreted in the opposite fashion, and it is impossible to completely wring out the self doubt from this process, nor should it be.
Surgery, then a Plan
Right now, we know that there are two lesions that need to come out, and we are headed back to Memphis for another resection with Dr. Boop on Thursday (first case, just the way I like it). While Dr. Merchant expressed some pained confidence in his assertion that we would find widely disseminated disease, the only way to really determine that is to take a look, try to remove what is visible, and then make a decision based on those findings.

We see CSI as being a salvage therapy, not an attempt for durable remission, despite Dr. Merchant’s declaration. I was able to grab Dr. Kun, another radiation oncologist at St. Jude who happens to be a little less gung-ho about CSI than Dr. Merchant, and he agreed that it would be a reasonable approach to buy Colin quality time. However, we still feel that stereotactic radiosurgery could give us more very high quality time, with the potential for some magnification of that time through the abscopal effect and the immunotherapy. CSI could still potentially remain as a further salvage option, depending on overlapping fields and so forth. There is another immunotherapy trial at MD Anderson that is intriguing, though it’s currently on hold while they wait for the third patient to reach a certain milestone in order to get the go-ahead from the FDA to move up to the next dosage tier. There are certainly other things we could try and may be useful tools, but the list of those that offer a scrap of hope of durable remissions is vanishingly short (read: zero).
At this point, we have a strategy but not a concrete plan until after surgery. We don’t even know how difficult the surgery will be or what the recovery time will be; ventricular tumors are the easiest to remove, so we know the procedure itself isn’t necessarily perilous, though it may bring dire news. This is the most up-in-the-air we have been since those early days, though without the comfort of knowing that we could reasonably go all in and take aim at the long view.
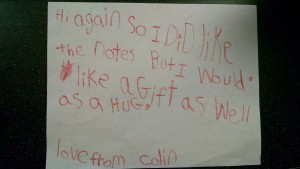
It is hard to write this without appearing morose. We do, in fact, remain hopeful in so many regards, and hope has a way of morphing to fit the situation. We see the joy in this dear boy who has lived the bulk of his life on borrowed time. We have no regrets for the way we have shaped the life around him. The other day, driving home from summer school therapy, Colin chirped from the back seat, “I’m really happy with the way my life is going.” He loves his new house in Ithaca, his friends, Northeast Elementary, and the wonderful community around us.
Maybe, just maybe, he will pull out of this in singular glory, but that doesn’t need to happen in order for us to view him as a miracle and his life as a resounding success. If not, he may even have years ahead, though this is also something we can’t bank on. We have to prepare for the full spectrum of contingencies because he deserves our thoughtfulness and he deserves to get the best out of whatever trajectory he ends up following in the days, weeks, and months ahead.
We will update on the results of surgery and the ultimate decisions about treatment, which may take some time to unfold, as they will require careful consideration of the previous field of radiation, the intended target with the new lesions, and how all that would affect the possibility of future CSI. Already, we have received much love and support from the community of everyone far and wide who rallies around Colin. It is the most basic sustenance of life, and it feeds us all.
I am so very sorry you, Colin and your entire family is going through this. It is just heartbreaking! Storming heaven with prayers for Colin!
Such an inspirational approach to all your family is going through, and already have overcome. The incredible love in these words, and what is not spoken, truly opens my heart and I am certain many others.
Peace and love to you all,
Mike Huber
Sending you all my love and prayers. Beautiful words, incredible family.
Hoping and hoping. Love you all.
I am in awe by your quality of perception and humbled by Colin’s personal awareness. For me, your efforts express all of the best qualities of our human situation when challenged by inexplicable life circumstances. The peace necessary to think and act so lovingly for Colin is a blessing that I am sure he feels. Much supportive love to you, Colin and the family.
Tamiko and Ian,
These are hard decisions, so many uncertainties and so many options. I am so proud of the way you are handling things. Your efforts to understand Colin’s condition and evaluate the options show you love for Colin and your whole family.
Love and prayers, Diana
I remember Colin after his first surgeries. It stinks that he has such rotten luck. We will be thinking of him and praying. Cancer sucks!
After reading again I am left breathless scared hopeful and in love with Colin…I am praying for success on all fronts