The children of St. Jude are now asleep, comatose in the aftermath of an orgy of candy consumption. Halloween is the biggest holiday here, bigger than Christmas (when the doctors presumably arrange for many of the patients to return home). This year’s celebration was toned down, presumably from infectious disease concerns; inpatients and outpatients were not allowed to intermingle.
The solution to the separation of the populations was “reverse trick-or-treating,” in which staff from the various areas roamed the halls, handing out candy to children in inpatient rooms. After this one-hour distribution of sugar, the inpatient children were allowed to go to the two inpatient wings on the second floor and, we had been told, a stop on the third floor (outside of ICU), though we forgot about that completely.
Of course, the celebration isn’t just about candy, but the decorations are elaborate, themed, and coordinated with costumes. In Halloweens past, Solid Tumor (2 South, the area where Colin stays inpatient) has often won the decorations category. However, another big disruption this year was the elimination of the decorations category. Instead, the departments competed on “child friendliness” and costumes.
This change and limits in the extent of the decorations, out of newer concerns for fire safety, created some anxiety in our unit. Much of the work leading up to the event was done by night nurses, but there were times when window painting ground to a halt because of higher intensity patient care duties. As time got tight, nurses and even their family members came in on their own time to paint the patient room windows.
The theme here in Solid Tumor was “Seussville,” so each patient room featured pictures and text from a different Dr. Seuss book. The staff assumed different Dr. Seuss personas, from Thing 1 and Thing 2, to green eggs and ham (Colin’s beloved nurse Kristen was the latter and pregnant Morgan, with her belly representing the yolk, was the eggs), to the Cat in the Hat and others. In desperation and in keeping with the theme, I put on blue pajama pants with stars, inverted a blue t-shirt, stuffed the belly a bit, cut out a paper star for the center of the belly, and drew a face with whiskers on a blue mask (star-bellied sneetch). Dad had found a doctor costume at Target, which I personalized with “Department of Hugs & Kisses” on one side. After his name tag fell off, he wrote “Dr. Daddy” on the other side.
Part of the idea was to make the medical environment less scary for Colin, who otherwise had enjoyed a poke-free day on Thursday and benefitted from a hiatus from procedures. Ironically, the doctor costume is the one we could most easily have assembled from materials at hand (real stethoscope, OR scrubs, etc.).
At St. Jude, nobody dresses as anything vaguely medical. The Seuss theme was big, especially since Leukemia (2 North, the inpatient area that mirrors Colin’s wing) chose the Grinch that Stole Christmas. It was charming and lent itself to some cute costumes, such as Cindy Lou Who, whose hair was done up perfectly (and stayed that way!).
Colin’s outpatient clinic evidently won the most child-friendly category. It was a garden/nature theme, with a profusion of crepe paper flowers. The staff dressed as insects, with Dr. DeWire appearing as Mother Nature, though she was mistaken by some as the Statue of Liberty. Another of the fellows, Dr. Wright, was a flower in a pot and wore an actual plastic pot around her waist.
The clinic that adjoins Brain Tumor won the costume category. They picked Charlie Brown and made actual papier mache heads for the costumes. It was very cute though hard to maintain since the heads, we were told, were very hot.
In addition to the clinics, other departments had tables, either in front of their offices or in random locations. The themes included: Egyptian (including mummies; children got their candy inside the pyramid); fishing; schoolhouse (by the St. Jude schoolteachers, who were surprised that Aidan picked a pack of binder paper instead of candy); Ghostbusters; Hollywood (they had a wall of fame with pictures of clinicians and walk of fame with names); Oz; Zoo Boo (there is a Zoo Boo event at the local zoo); cruise; winter wonderland (the various rehab disciplines; we had to ask our physical therapist if she was wearing a costume or just an outfit – only the sparkly makeup was unusual); wild west; pirates; breakfast cereal (seriously. And they gave out small boxes of heavily sugared cereal instead of candy); Willy Wonka and the Chocolate Factory; medieval castle; pixies; Winnie the Pooh; Ratatoille. I am probably forgetting some or didn’t even see them.
The crowds were thick though not crushing, but still enough to get Aidan in a panic. Initially, we had been told that siblings of inpatients would have to stay in the inpatient areas but then were told that we could have clearance for full access. Also, we had heard that security guards would be manning the stairwells and elevators to monitor activity, but this never came to pass.
As for Colin, all of this was almost entirely moot. After the debacle of venous access on Wednesday, we offered our team the option of either allowing us to participate in rounds or not performing any procedures on Colin for the day. Our concern was really that Colin clearly had had enough and needed a break. If the team wanted to do anything, we felt it was necessary for his voice to be heard (i.e. let us participate in rounds so we can pipe up on his behalf).
Of course, we also knew that they would never open the door of the medical sepulcher. We have already asked to participate in rounds in the past, with the response of deafening silence. Although it is not common practice, it is done at some other hospitals and HIIPA-related concerns can certainly be overcome. But this is one area where St. Jude is not going to be easily swayed, and the entire goal was that the team recognize that Colin needed a respite.
The medical outcome came as no surprise. Although the PICC had been delayed previously because of the positive peripheral culture, the pressing need to get a good vein on Colin overrode the Infectious Disease protocols, and we scheduled the installation of the PICC. (Here is a vague but adequate description of the three types of central lines that we have discussed, including illustrations.) In addition, the team wanted to take another look at Colin’s heart, this time with a trans-esophageal echocardiogram (TEE). Because we were trying to coordinate the two procedures back-to-back with a day’s notice, the latter seemed impossible, but Andrea, the nurse practitioner, worked miracles and convinced the cardiologist to switch his schedule around to accommodate the narrow window available.
For most of Thursday, we assumed that we would have to simply resort to a repeat thoracic echocardiogram, knowing that the last had revealed no vegetation and ambiguities regarding a venous catheter. Without the lungs in the way, the cardiologist would get a much better view and more definitive reading.
On Thursday morning, after a day without any invasive procedures (even so, Colin curled up defensively, even when approached with something as benign as a stethoscope), Colin went in for sedation for the TEE. Because he has a trach, they were able to begin sedation with the least amount of anxiety to him, simply pumping an agent into his trach. Even so, he panicked a bit when transferred into the crib for the procedure and got a big hug until he was limp and sleeping.
Dr. Joshi 1, the cardiologist, was able to provide his interpretation of the TEE very quickly. The exam itself took only 10 minutes, and then Colin was free to move on to part 2. However, we found out that Colin does in fact have “vegetation” on one of the heart valves. Also, the object which had previously been read as a central line catheter is actually a fibrin sheath that had formed around the catheter, creating a ghost impression of the old catheter.
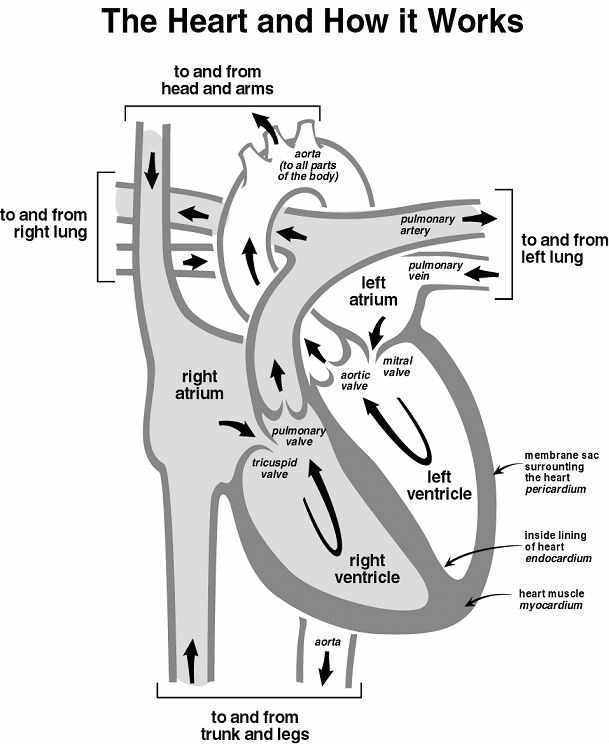
Interestingly, the “vegetation,” which apparently looks like aquatic vegetation, grows on the side of the valve right atrium directly opposite the tip of the catheter, implying that it grew where the stream of fluids from the old port shot out.
This finding supports the idea that Colin’s fungemia is a recurrence of the old infection, which had evidently lain dormant on a heart valve but flourished in the presence of the rich environment of the IV nutrition. The interventional radiology team, headed by Dr. Joshi 2 (he is really the original Dr. Joshi, since he installed Colin’s G-j tube several weeks ago) did not want to install the PICC line, instead preferring a femoral artery line that would be more robust than the peripheral lines we had been struggling with.
However, based on concerns regarding infection (a femoral line is in the diaper area), Dr. Gajjar asked for the PICC. Infectious Disease has acknowledged that we absolutely need to deliver IV medication, namely the micofungin. We will perform periodic cultures, especially to determine if the PICC has become infected (this is the reason that interventional radiology didn’t want to put in the PICC).
There is no perfect solution to this problem, but Dr. Gajjar has to perform air traffic control and make a definitive decision, one that he feels is in Colin’s best interest. He and Dr. DeWire have a much better understanding of Colin’s treatment arc and what he will be needing over the next few weeks and months. Both doctors came to see us on Thursday and provide a united front, letting us know that they are firmly in command of Colin’s ever-complicated case. There is a sense that his care can too easily get muddled by a multitude of practitioners. Therefore, in order to reduce clutter, they want to make sure that he has a single specialist physician who follows him in each area rather than multiple doctors from the same group.
We sense that Dr. Gajjar thinks it is also too confusing for us to hear directly from other disciplines what they want or what they think ought to be done. There is definitely truth to this, as the I.D. fellow told us earlier than Colin had had a different candida infection in New York and that he has an enlarged heart but it is nothing to worry about (the cardiologist, who had also seen the earlier cardiogram, later explained that this is a common adaptation in children with anemia). Also, I.D. said that Colin will have to have two peripheral cultures a week until he is clear, eliciting more anxiety on our part. I fretted about making sure that these are coordinated to take place when Colin is sedated for other procedures in order to save him the stress.
However, Dr. Gajjar has made it clear that Colin will have cultures done when it makes sense to his holistic care and is not beholden to I.D.’s schedule (phew!). The most productive aspect of all this has been to gain a better appreciation of the role that our team plays in balancing the various risks and benefits from a wide circle of specialists. We obviously need to keep an eye on the integrity of the PICC line, which will hopefully last until he can get a permanent device installed.
Now that he has good venous access, we have resumed discussions on chemotherapy. There is no reason to delay because there is no specific change we are waiting for, Dr. Gajjar explained. Thus, assuming that Colin does well clinically and medically over the next few days, we will start the third cycle of chemo on Tuesday.
Colin is already much better, though he was a bit too groggy from his procedures to enjoy trick-or-treating and refused to wear his Lightning McQueen costume (he perked up later and was very flirty with Dr. DeWire and Kristen, his nurse). Aidan accumulated a bag of candy too large for him to carry and has been politic enough to raid it out of Colin’s view. Colin seems less distressed by others eating (it helps that the rate of his feeds has been steadily increasing since he lost IV access), though he does love candy, especially chocolate.
There is no such thing in Colin’s world as an absolute failure, just as many of his successes are tempered by complications. Despite his recent setbacks, Colin continues to improve in other ways and has begun doing something in physical therapy that he had not done previously (pushing himself from leaning over back to sitting). His awareness of his situation is stressful but also encouraging, because it means that his mental state is much improved.
We are also lucky to be supported by people wherever we go. Back home, a family cleaning crew has been working on an infestation that is probably worse than the one Colin is currently battling. Let’s just say that we were not able to suppress the growth of any suspected pestilence before our departure but knew that our cupboards would have to be pretty much emptied.
Here in Memphis, a family from school went out and got Aidan a Halloween costume (and a very cute themed throw) when we were unable to set aside the time. Thus, he was able to roam the halls as a king (last year, he was a knight, so he must have gotten a promotion. As an additional aside, one man asked if he was the Burger King; when a group of ladies asked him what he was king of, he replied “cheeseburgers.” For some reason, the mistranslation was even better received than the original would have been). We have also gotten help from a family at Aidan’s school whose daughter is a St. Jude brain tumor survivor. She even went to Boston for proton therapy. The volunteers here are a constant source of support, both when they stay with Colin so the rest of us can be together and when they listen to our story or even just see how much better Colin is doing. A number of volunteers are former St. Jude patients, and there is one I know of who is the parent of a former patient.
People want to help and they do, whether they know it or not. We appreciate that people are following our family’s adventure. I used to use the word journey until I met a patient here, a little girl, who told me in a weary voice that her mom named her caringbridge site using the word journey. What would she have preferred, if she had named it? Adventure. There is much more promise in adventure than in journey, and it seems less arduous.
Even in the face of difficult decisions or situations, there are worse things than this. For one thing, there are more challenging cases and more obstinate diseases. There is a family here with a little girl with a diffuse brainstem glioma who is deteriorating before their eyes; in three weeks, she went from diagnosis to paralysis on one side of her body. At six, she can no longer speak. There are new drugs that may help, and her parents are willing to try what they can with the hope of curing her or, in the face of failure, contributing to the understanding of that disease.
Not so long ago, leukemia was considered incurable and the patients here with brain tumors were the “lucky ones.” Now, the statistics have reversed, but advances in medicine and our understanding of cancer open the door to better cure rates and treatments with fewer long-term side effects. We are already the beneficiaries of these things and are fortunate enough to be getting treatment in an environment where we get both advanced cancer treatment and medical care that is provided with no concern for insurance approvals or cost. The absence or presence of financial concerns affects medical care itself, not just the families who are ultimately on the hook for the bill.
If Colin’s fungemia is the trick, then the treat is knowing that he is getting the care he needs from a team that is fully focused on doing what is right for him.
If one of the three is inhibited at all, I’m guessing it might be least threatening for it to be the tri-cuspid wot? what good timing, to have this problem post-FDA approval of the newer anti-fungal!! He just continues to be a talented and gifted patient!
rwh
As you describe your adventure, I’m reminded of the recurring theme in The Lord Of The Rings of “help un-looked for”. There are times when our adventurers seek out help and they find it, other times when they seek it and are denied, and sometimes help just appears, out of the clear blue sky – like the Eagles.
Here’s hoping that the help you need finds its’ way to you.
PS – testiness about costumes is not limited to boys who’ve been feeling like pincushions. Believe me, I know.
I want to introduce myself to you all. My name is Jeff Marshall from Brookfield VT. I was made aware of Colin by Mark through Team Helix Folding@Home. Colin has been in my prayers since I first heard about him, and he will remain in my prayers, thank you for this opportunity.
Mark, it was great that you were able to come and help out. As I mentioned in the post, we get help from so many people in so many ways, and we are grateful that you were able to break away and give us that time while I was out of town. Because of the logistical difficulties when I travel, we’re not planning on a repeat while Colin is going through chemo. Thanks again!
I heard of the large effort over at your house back home. It’s cool how I was there trying to do something useful while they were up there definitely being helpful.
I hope Colin was not upset about me leaving, as well I hope Aiden wasn’t hurt either.
I remain ready and willing to come back down there more times to chip in and any suggestions on how I might do anything better I am all ears.
Please tell Colin and Aiden that their uncle loves them and tell Aiden he doesn’t have to take a goodnight kiss or hug if he doesn’t want to, I just want him to know that he and his brother are very precious to me.
Bless you all, Bless the doctors, and bless the staff there and at Target house.
Nobody specified the valve, but they did specify the chamber (right atrium), implying the tricuspid valve, as far as I can tell. Fortunately, the vegetation is “small,” according to the cardiologist. Also, this condition, technically “endocardiosis,” is quite unusual here. We understand that the I.D. attending who has been here for 27 years has seen a handful of cases (literally on the order of five), with fewer of these due to fungemia.
As always, our boy has a knack for beating the odds!
We are lucky for advances in medication for fungal infections and St. Jude’s enthusiasm to use this expensive but effective and well tolerated medicine (it is so well tolerated that it can be used during chemo; Ampoteracin B, which used to be the biggest gun in the arsenal, is incompatible with chemo because it is too toxic). Colin may need to take it for six months, with a minimum course of six weeks or so (dated from the last negative blood culture).
T: As you know. I am a cardiology enthusiast; whereas the three valves in the heart are each strategically different portals of blood flow to very different aspects of Colin’s physiology, your having told us “a heart valve has become a nesting place of fungal habitation” (sic), inspires an interest in learning which of the three valves is so corrupted – as that particular part of his hemo-aqui-ology will be the more impeded by the friction of the vegetation, as well as the restriction of tactile flexibility of the valve in question. This casual reference (a valve) suggests to me that this particular valve’s logistics must be useful information in pursuing Colin’s life support. When you speak with the wizards, you might ask? Which valve?
Pop